It’s can be pretty terrifying when your doctor calls you up and tells you the results of your MRI or advanced imaging are in. You rush over to him, eager to find out if there is something to explain your back pain. He then tells you some big words you can’t understand, let alone pronounce, and you leave feeling like you’re broken.
<strong”>Well, I’m here to tell you that you aren’t broken. More often than not, the results of your imaging are irrelevant in getting you back to full function. The findings of your imaging do not mean you get to slack off and stop working hard. Sorry, but if you’re looking for someone to tell you that rest is the best medicine and will heal all, you’ve come to the wrong place.
The Human Body and Our Natural Ability to Heal
The human body is an incredible thing. Incredible in all it does, but also incredibly variable. For example, did you know the sciatic nerve is above the piriformis muscle in some people, below the muscle in others, and actually pierces the muscle in the rest of us? Or that cadaver studies show the latissimus dorsi can actually insert in a completely different place in some individuals?
And when it comes to the back, did you know that some people have an increased curve in their spine, some have scoliosis, and some actually have an extra vertebra? On top of that, lots of people have disc degeneration, vertebral fractures, and disc herniations, while many others have none of these things.
The point I am getting at is simple: our anatomy is not perfect and not uniform. But that does not mean it is wrong or that it is problematic. These things may not be any cause for concern or at the root of our pain.
This is the part that can be hard for some of my clients to believe – just because an X-ray, CT scan, or an MRI shows an “abnormality” does not necessarily mean you are abnormal or that you need fixing. It may not mean anything is remotely wrong or needs to be addressed. Because for many people, the “abnormality” discovered is simply their normal.
An illustration of “normal” disc anatomy, but that’s all it is – an illustration.
Dealing With Test Anxiety
I often have clients come to me after having had advanced imaging done, and they are anxious, terrified, and upset from what they “have.” Moderate degeneration, a large disc bulge or herniation, spondylolisthesis – all of these big, scary words that sound so daunting. Things that have been labelled as the reasons for their pain.
“Unless the situation is so bad that surgery is the only option (and this is extremely rare), treatment follows the same path[.]”
But here’s the thing: while it might be the reason for the pain, a lot of the time it really isn’t. To be honest, these findings are not all that meaningful in determining the issue at hand – the real cause of the pain. What is meaningful are the person’s symptoms and the physical findings from an assessment – general movements, mobility, strength, nerve function, and physiological and non-physiological movements.
Simple stated: you are not the results of your MRI. Your pain is not necessarily coming from any findings on your imaging.
But What Does the Research Say?
A study published in the New England Journal of Medicine in 1994 looked at 98 asymptomatic (healthy, pain-free) participants, using an MRI to look at their spine. 82% of those MRIs were positive for a disc bulge, protrusion, or extrusion at one level, with 38% actually having these issues on more than one level.
An even more recent study published in 2014 showed the percentage of “abnormal” findings on a lumbar spine MRI and CT images in healthy, pain-free individuals. Check out the results in the graph below that I created based on the study results. I encourage you to really, really look at this graph.
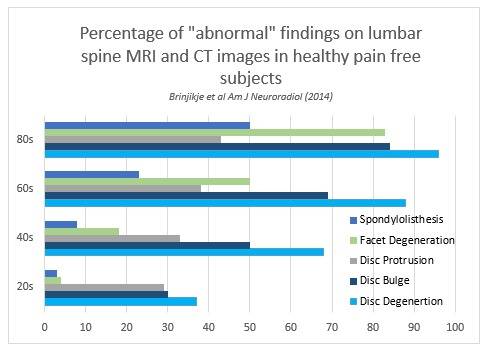
If you take a look at individuals in their forties you will see that almost 70% of these healthy individuals had disc degeneration, 50% had a disc bulge, over 30% had a disc protrusion, and still more had spondylolisthesis and facet degeneration. Those numbers are huge, and shed light on the fact that we cannot be using imaging alone to make clinical diagnosis and treatment plans.
What Does This Mean?
Put simply, this research means there are people out there with back pain who have no abnormal findings on imaging and there are people out there with abnormal findings on imaging with no back pain. Furthermore, it means some people have both back pain and abnormal findings, but often the two are unrelated.
Confusing, isn’t it?
This means that though advanced imaging is absolutely important, it is not clinically significant in many cases. The problem is people get these results and automatically equate their pain to the “abnormalities.” Unfortunately, both clinical experience and the aforementioned research show us that imaging does not improve clinical outcomes. In other words, it does not improve treatment, recovery, or function.
“More often than not, the results of your imaging are irrelevant in getting you back to full function.”
In fact, most good physical therapists and chiropractors will not look at the results of imaging before assessing their clients because they don’t want the results to bias their assessment. Said another way: you should never treat an MRI – you should treat only a person.
We as therapists have the means to determine what is clinically significant and where the pain is stemming from. If someone comes to me with back pain and an MRI that says she has a disc herniation, but my provocation test isn’t positive, then chances are her pain is coming from something entirely different than that herniation.
Does Any of This Even Matter?
Here’s the kicker. Most of the time the answer is no, it does not even matter. Whether it’s degeneration, disc bulge, herniation, or a back issue you just can’t seem to figure out -treatment really doesn’t change too much. Unless the situation is so bad that surgery is the only option (and this is extremely rare), treatment follows the same path: pain and symptom relief, exercises, restoring full function, and preventing future recurrences.

Stretching and soft tissue work are some of the many tools we use in the rehabilitative process.
Pain relief for any of these issues might include traction, soft tissue mobilization, manual therapy, and/or stretching. Exercises for all of these issues will include core stabilization and general strength. Restoring function means getting people back to living their daily life, and having the strength and mobility to do so. Preventing future recurrences means correcting any imbalances and maintaining good mobility and stability.
So, you see, it doesn’t matter what results we find. We treat the person. We don’t treat the MRI.
Conclusion
If you have a back injury, don’t freak out when you hear your MRI results. Remember this article. Remember that graph. You are not the results of your MRI and those big, scary words cannot and should not stop you.
Maybe the abnormalities found are really your normal. Maybe they have nothing to do with your pain. But regardless of if they do or don’t, you will still be okay. Just make sure to work with a professional and treat your injury and symptoms, not your MRI.
Check out these related articles:
- Myths About Disc Bulges: They Are Not Forever – But Training Is
- The Rabbit Hole of Back Pain – What Your Doctor Doesn’t Want You to Know
- A Case Against Ultrasound In the Treatment of Injury
- What’s New On Breaking Muscle Today
References:
1. Brinijiki, et al. “Systematic literature review of imaging features of spinal degeneration in asymptomatic populations.” American Journal of Neuroradiology (2014) 36(4): 811-816.
2. Jensen, et al. “Magnetic Resonance Imaging of the Lumbar Spine in People without Back Pain.” The New England Journal of Medicine (1994) 331:69-73.
Photos 1 and 2 courtesy of Shutterstock.
Photo 4 courtesy of Shannon Khoury.






