By now it should come as no surprise that there exists a very serious worldwide obesity epidemic. After all, television’s hit show “The Biggest Loser” is centered around people whose weight has become a real problem—emotionally as well as physically. These individuals then compete to lose as much weight as possible, with some losing several hundred pounds over the course of a few short months (contestants are typically involved with the show for anywhere from 3-5 months).
The most recent statistics would suggest that nearly 2 billion adults worldwide are overweight. 500 million adults worldwide are estimated to be obese. When children are added into the statistics, we see obesity rates start to top 40% of the world’s current population. Extrapolating from this data, it has been projected that by the year 2025, over 40% of all adults will be obese.
The global obesity epidemic is one of the greatest public health challenges faced in the 21st century. Morbidity and mortality rates are rising significantly with no end in sight. The ready availability of high-calorie food combined with sedentary lifestyles has become a potent recipe for a health crisis. Individuals that are overweight and obese face serious health consequences including cardiovascular disease, type 2 diabetes, osteoarthritis, sleep apnea, musculoskeletal disorders, and some cancers. If this trend continues, there may come a tipping point where twentieth century gains in life expectancy could be reversed.
Strategies for the Obesity Epidemic
The medical options for treating obesity are limited, costly, and carry significant risks. Gastric bypass is one effective surgical treatment, with post-operative follow-ups showing as much as a 92% reduction in diabetes deaths, 60% reduction in cancer deaths, 56% reduction in coronary artery disease deaths, and 40% reduction in other obesity-related deaths. However, gastric bypass surgery carries a mortality rate of 0.5%.1,2
Lifestyle modification strategies (diet and exercise) currently form the main treatments for obesity. However, results are generally disappointing, and the majority of people who attempt this strategy regain any lost weight within 5 years.3
Effective treatments to combat and eventually prevent the growing obesity epidemic are contingent upon developing a better understanding of the processes that regulate body weight. There is an apparent disruption within the hormonal and biochemical pathways of overweight and obese individuals. There also appears to be a disconnect between various brain regions that regulate both appetite and reward behaviors. Recently, there has been a tremendous interest in, and focus on, the connections between the gut hormones that are secreted after eating and these same brain regions. Also of interest has been how exercise may accentuate the effect of these hormones and their role in satiety before, during and after strenuous activity.
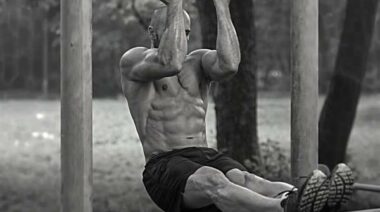
Effective treatments to combat obesity will require a better understanding of appetite. [Photo credit: Sandra Cohen-Rose | CC BY 2.0]
Gut Hormones and Weight Management
The gastrointestinal (GI) tract is the body’s largest endocrine organ. The chemicals produced and secreted by the GI tract play substantive roles in satiety, energy intake, and energy output. The most-examined hormone in this area is peptide tyrosine tyrosine (aka pancreatic peptide, or PYY). PYY is a short (36-amino acid) peptide released by cells in the ileum and colon in response to eating. PYY is also produced by a small group of neurons in the brainstem. These particular neurons can be found in the medulla oblongata, home to the vagus nerve, which is also involved in feelings of satiety after eating.
PYY’s primary role is to reduce appetite, the psychological component to eating. It also plays a very important role in the regulation of energy balance in the body. Higher levels of PYY lead to a reduced calorie intake, provide a buffer against diet-induced obesity, reduce appetite (the psychological side of eating), and aid in weight loss. Conversely, low levels of PYY lead to feelings of hunger and enhanced cravings, while simultaneously predisposing a person to retain fatty tissue. Functional brain imaging techniques have also shown that elevated levels of PYY affect brain regions—the hypothalamus and brainstem—involved in reward processing.2 Specifically, if levels of PYY are high, these brain centers show increased activity, suggesting the brain feels satisfied or rewarded, and thus cravings are reduced.
How PYY Works
PYY works by slowing the emptying process of your stomach and intestines. Therefore, it increases efficiency of digestion and nutrient absorption after a meal. PYY also increases water and electrolyte absorption in the colon. The combination of these actions leads to feelings of fullness that last longer. PYY may also suppress pancreatic secretion, which in turn will reduce insulin levels in the blood. This also reduces appetite and controls calorie consumption. Additionally, a reduced level of insulin will prevent, or at least limit, fat storage.
PYY is released by the stomach in a nutrient-dependent manner. Concentrations of PYY are influenced by the amount of calories consumed, the macronutrient composition of a given meal, and by the consistency of the food consumed. PYY levels increase after food consumption and decrease during periods of fasting. After eating, PYY levels rise within 15 minutes, and reach a steady peak level within approximately 90 minutes.
The consumption of a protein-rich meal has a significant effect on PYY levels. This serves to further reinforce the notion that consuming a higher protein diet can be beneficial to weight loss. After consuming a meal higher in protein, PYY concentrations are typically elevated resulting in greater feelings of satiety. Equally important is that high-protein meals cause a secondary and delayed release of PYY, which will prolong feelings of fullness after eating. This is why high-protein diets have been recommended to help certain individuals reduce hunger while promoting weight loss. Elevated PYY levels also appear to prompt individuals to reduce their consumption of higher fat foods.1,2
PYY and Energy Consumption
While PYY clearly plays an important role in energy consumption, less attention has been paid to that function. There is increasing evidence that PYY has beneficial effects on metabolism, energy expenditure, and substrate partitioning as a fuel source, as well as for storage purposes. Higher PYY concentrations increase basal metabolism, increase fat breakdown and improve insulin sensitivity.
Low PYY hormone concentrations have been associated with higher BMI levels and waist circumferences. Both of these metrics are positively correlated with increased morbidity and mortality rates. Low levels of PYY hormone have also been correlated with a lower resting metabolism. Resting metabolism accounts for the greatest proportion of daily energy expenditure, and plays a huge role in regulating body weight as well as body composition.
Recently, the research community has looked into the role of high-intensity interval training (HIIT) and its effects on food intake. It has been demonstrated that 12 weeks of HIIT leads to increased levels of PYY hormone, which in turn causes individuals to consume less calories than those performing low-intensity cardio.4 It appears that PYY hormone production is elevated, and appetite is depressed, by higher intensity exercise. This could prove to have major implications when looking for appropriate treatments for overweight and obese individuals.
New Strategies for the Obesity Epidemic
The global obesity epidemic has escalated the need to discover new strategies to counteract it. Traditional lifestyle modification alone—light to moderate activity coupled with dietary adjustments—has proven relatively ineffective in modern, Western society. This is largely due to the abundance of high-calorie, low-cost food, coupled with a predominantly sedentary lifestyle. The development of bariatric surgical techniques over the past decade is a major breakthrough in treatment for the very obese, but it is not without drawbacks. It carries risk, cannot be tailored easily to individual needs, and does not address the needs of hundreds of millions of people who do not meet the requirements for the procedure, yet who remain at significant risk.
Exercise is available to everyone, whether in a health club or at home. Intensity of exercise may be a key element to unlocking the benefits of PYY. Although potentially controversial, it may be necessary to get overweight and obese individuals to start participating in exercise regimens like CrossFit and HIIT. The intensity associated with these routines can be leveraged to capture benefits that more than compensate for the inherent risks found in any exercise routine.
Your crash diet won’t help you:
References:
1. Batterham, Rachel L., and Stephen R. Bloom. “The gut hormone peptide YY regulates appetite.” Annals of the New York Academy of Sciences 994, no. 1 (2003): 162-168.
2. De Silva, Akila, and Stephen R. Bloom. “Gut hormones and appetite control: a focus on PYY and GLP-1 as therapeutic targets in obesity.” Gut and Liver 6, no. 1 (2012): 10-20.
3. Anderson, James W., Elizabeth C. Konz, Robert C. Frederich, and Constance L. Wood. “Long-term weight-loss maintenance: a meta-analysis of US studies.” The American Journal of Clinical Nutrition 74, no. 5 (2001): 579-584.
4. Prado, Wagner Luiz, Mara Cristina Lofrano-Prado, Lila Missae Oyama, Michelle Cardel, Priscyla Praxedes Gomes, M. L. Andrade, C. R. Freitas, Prabhakaran Balagopal, and James O. Hill. “Effect of a 12-Week Low vs. High Intensity Aerobic Exercise Training on Appetite-Regulating Hormones in Obese Adolescents: A Randomized Exercise Intervention Study.” Pediatric Exercise Science 27, no. 4 (2015): 510-7.