As trainers, we must understand that every body is unique. Not everyone will have the same bone structure, morphology, or physical capabilities. Some people have ailments that we must address so we do not hurt or cause any more harm to them. This series is to help coaches grasp different populations that have ailments that plague them everyday, but still have the desire to exercise and stay healthy.
As trainers, we must understand that every body is unique. Not everyone will have the same bone structure, morphology, or physical capabilities. Some people have ailments that we must address so we do not hurt or cause any more harm to them. This series is to help coaches grasp different populations that have ailments that plague them everyday, but still have the desire to exercise and stay healthy.
Science of Fibromyalgia
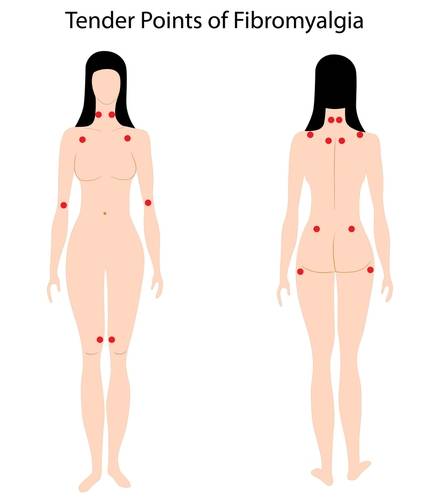
Fibromyalgia is a muscular disorder. Fibromyalgia syndrome (FMS) is associated with elevated systemic and inflammatory biomarkers and an innate cellular response mediated by monocytes and neutrophils. So, that is the basic definition, but what exactly is it and how does it affect those who suffer from it?
FMS affects up to 3% of the population and women comprise about 85% of those diagnosed. Many believe this is because males are less likely to see physicians about symptoms that may be related to FMS. FMS is different in that it is not a viral, bacterial, or fungal infection. It is not autoimmune like rheumatoid arthritis or lupus. Rather, some suggest it is a complicated combination of related sleep disorders, endocrine and neurotransmitter imbalances, and possible emotional state.
Sleep Disorder
Sleep studies done with FMS patients indicate that they seldom or never enter the deepest level of sleep, stage IV sleep. It is in this stage that adults secrete growth hormone, the hormone that stimulates the production of new cells and collagen for healthy recovery. This may be the reason why fibromyalgia patients have difficulty recovering from hard workouts. Along with this, not getting adequate, high-quality sleep reduces serotonin levels and serotonin helps modulate pain sensation. Many FMS patients report getting an average eight hours of sleep, but feel unrefreshed, as though they have been up all night.
Fatigue
Poor sleep may not be the only cause of fatigue in FMS patients. Some research suggests FMS involves a problem in mitochondrial function: phosphates accumulate in the muscle cells rather than attaching to adenosine to form adenosine triphosphate (ATP, remember the powerhouse of the cell?). This leads to problems with energy production and with calcium reabsorption. This results in inefficient muscle contractions and fatigue.
Pain
This is still being studied in the medical community for FMS patients. Some studies suggest the pain is not actually generated in muscles, as the syndrome name implies. Instead, examinations in the cerebrospinal fluid of FMS patients show pathologically high levels of two neurotransmitters, substance P and nerve growth factor. These substances are believed to initiate nerve activity, cause vasodilation, and increase pain sensation.
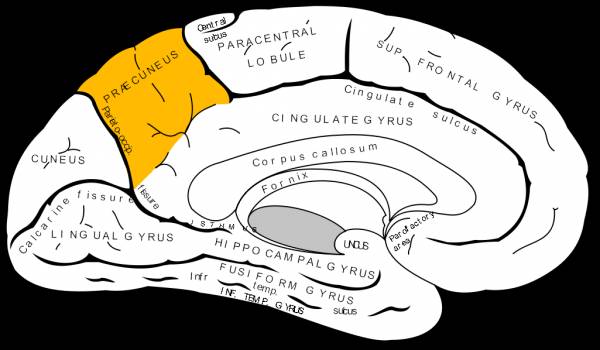
Studies have also been done as far as structural alterations in FMS patients in the brain stem that makes them sensitive to mechanical pressure. To test this, researchers in the UK evaluated the geometric differences in subcortical structures in FMS patients. In the study, sixteen female FMS patients and fifteen others age and sex matched for the control were used. The healthy control group underwent high-resolution T1-weighted magnetic resonance image scanning. The data was analyzed using the control with FMS patients. It was concluded the FMS patients exhibited alterations to the shape of the left lateral aspect of the lower brainstem (the medulla). The mean total volume of the brainstem was significantly reduced in FMS patients versus the control. It was also identified that FMS patients had decreased local grey matter volumes in the brainstem (pons) and left precuneus and increased grey matter volumes in the bilateral primary somatosensory cortices. These results indicate that these alterations in FMS patients may contribute to mechanical sensitivity or pain.
FMS and Exercise
There have been tests done to examine the physical fitness parameters of FMS patients versus healthy individuals. One test used 39 women with FMS and forty controls. The physical tests studied were maximal aerobic capacity, muscle strength and flexibility, daily physical activity, pulmonary function tests (PFTs), body composition, depression, anxiety, and health-related quality of life (HRQoL).
The results concluded that muscle strength, HRQol, depression, and anxiety symptomology were impaired in FMS patients compared to the healthy control group. Low muscle strength is related to reduced HRQoL and increased depression and anxiety in FMS patients. It is suggested that FMS patients perform daily exercises including aerobic and strength training as it may be beneficial to them.
Coach’s Corner
So, how do you work with a FMS patient? What works and what doesn’t? The most important thing is to get to know your client. Understand his or her medical history, and if he or she has worked out in the past, find out what initiated any flare-ups. Make sure you write these down; you do not want to repeat what made an FMS patient flare up to begin with.
It may help to have FMS patients be a bit more in control of the workouts in the beginning, as they are the ones living with the disorder. As the coach, if you feel what they are doing is too similar to unsuccessful past attempts at exercise, stop them and explain to them why it’s important to start slow.
Coaches who want to integrate resistance training with FMS patients need to think outside the box. You do not always have to start FMS patients with dumbbells, kettlebells, or barbells. You can start them with a basic resistance band or even bodyweight work until their body becomes accustomed to training. As FMS patients get stronger you can introduce other forms of resistance training.
As far as aerobic training, work with low impact in the beginning. Aerobic work like rowing, Airdyne, swimming, and even water aerobics work great in the beginning stages of fitness for an FMS patient. As the patient becomes stronger and more efficient without having flare ups, you will be able to introduce new ideas and equipment into the mix.
For Fibromyalgia Patients
There are other forms of exercise to look at when it comes to managing pain. Studies show that tai chi has benefits not only physically but psychologically as well. A study was conducted using twelve- and 24-week tai chi programs and examined acute pain as well as cumulative changes. Thirty-six patients with FMS participated for twelve weeks (three sessions a week), and 28 patients continued the program for another twelve weeks (making 24 total weeks). The study determined that tai chi programs decreased levels of acute pain in FMS patients. Tai chi is considered low to moderate exercise, so integrating similar things like water aerobics, gentle yoga (non-heated), and qi gong can be holistic ways to manage acute pain symptoms.
For some, FMS is debilitating. It’s important for coaches to understand what FMS is and the symptoms it can bring in a person with the condition. Many FMS patients feel if they start an activity too fast too soon that it causes them to flare up with symptoms, which can lead to excruciating pain. If done right, exercise can help FMS patients live whole lives without pain and with the added benefit of keeping them healthy.
If you are an FMS patient, make sure you let your coach know your symptoms, your past flare-ups, what triggers your pain, and if you are in constant pain. This is important information for your coach so they can create a training plan right for you. If you are new to exercise, you can try low to moderate forms of fitness as mentioned above. It’s important to not let the disorder rule your life. Instead, try to take charge of your life and live happy and healthy.
References:
1.Segura-Jimenez V and Romero-Zurita A, “Effectiveness of Tai-Chi for Decreasing Acute Pain in Fibromyalgia Patients,” International Journal of Sports Medicine. (2013): efirst, accessed December 2, 2013.
2. Fallon, Nicolas and Alghamdi, Jamaan et.al. “Structural Alterations in Brainstem of Fibromyalgia Syndrome Patients Correlate with Sensitivity to Mechanical Pressure,” NeuroImage Clinical. (2013): 163-170, accessed December 2, 2013.
3. Vincent, Ann and Benzo, Roberto P et. al., “Beyond Pain in Fibromyalgia: Insights into the Symptom of Fatigue,” Arthritis Research and Therapy. (2013): 221, accessed December 2, 2013.
4. Sener, Umit and Ucok Kagan et. al., “ Evaluation of Heath Related Physical Fitness Parameters and Association Analysis with Depression, Anxiety, and Quality of Life in Patients with Fibromyalgia.” International Journal of Rheumatic Diseases. (2013): efirst, accessed December 2, 2013.
5. Wener, Ruth. Guide to Pathology Third Edition (Baltimore: Lippincott Williams and Wilkins, 2005), 64-67
Photo 1 by Mikael Häggström By Mikael Häggström [Public domain], via Wikimedia Commons.
Photo 2 by Mysid Gray [Public domain], via Wikimedia Commons.
Photo 3 courtesy of Shutterstock.






